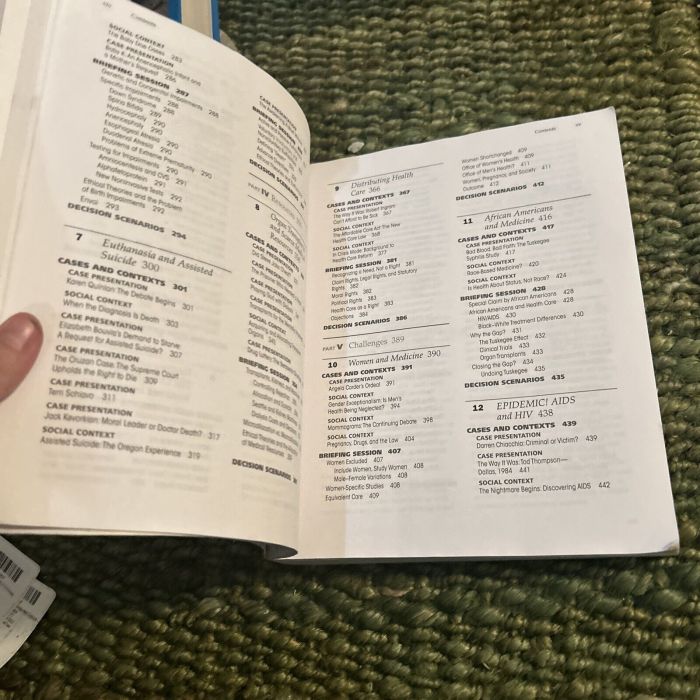
Intervention and reflection basic issues in bioethics 10th edition – Intervention and Reflection: Basic Issues in Bioethics, 10th Edition presents a comprehensive examination of the ethical principles and issues that arise in healthcare practice. This authoritative text provides a thorough grounding in the fundamental concepts of bioethics, empowering healthcare professionals and students to navigate complex ethical challenges with confidence.
Through engaging case studies, real-world examples, and expert insights, this book explores the ethical dimensions of medical interventions, decision-making, and end-of-life care. It emphasizes the importance of patient autonomy, beneficence, and ethical reflection in ensuring the delivery of compassionate and ethical healthcare.
Ethical Principles in Intervention and Reflection

Ethical principles serve as foundational pillars in healthcare practice, guiding decision-making and interactions between healthcare professionals and patients. These principles ensure the protection of patient rights, promote patient well-being, and facilitate ethical decision-making in complex healthcare situations.
Autonomy
Autonomy refers to the right of individuals to make decisions about their own healthcare, including the choice of treatments, refusal of interventions, and end-of-life care. Respecting patient autonomy is paramount in healthcare ethics, as it empowers individuals to exercise control over their own bodies and lives.
Beneficence
Beneficence is the principle of doing good and avoiding harm to patients. Healthcare professionals are obligated to act in the best interests of their patients, prioritizing their well-being and minimizing potential risks or harms associated with interventions.
Ethical Dilemmas
In healthcare practice, ethical dilemmas often arise due to competing ethical principles or values. For instance, a patient may refuse life-sustaining treatment, which conflicts with the principle of beneficence. Healthcare professionals must carefully navigate these dilemmas, considering the patient’s wishes, medical condition, and legal implications.
Ethical Issues in Intervention: Intervention And Reflection Basic Issues In Bioethics 10th Edition
Informed Consent
Informed consent requires that patients receive clear and comprehensive information about their healthcare options before making decisions. This includes understanding the potential risks, benefits, and alternatives of proposed interventions. Informed consent ensures that patients are actively involved in their own healthcare and make informed choices.
Confidentiality
Confidentiality is essential in maintaining patient trust and protecting their privacy. Healthcare professionals have a duty to safeguard patient information, including medical records, conversations, and personal details. This principle promotes a sense of safety and encourages patients to disclose sensitive information necessary for their care.
Decision-Making Capacity
Assessing a patient’s decision-making capacity is crucial in determining their ability to make informed choices about their healthcare. Healthcare professionals must evaluate the patient’s cognitive abilities, understanding of information, and ability to communicate their decisions. When patients lack decision-making capacity, surrogate decision-makers may be appointed to represent their interests.
Withdrawing or Withholding Life-Sustaining Treatment
Decisions regarding the withdrawal or withholding of life-sustaining treatment present significant ethical challenges. Healthcare professionals must consider the patient’s wishes, medical condition, and the potential impact on their quality of life. Ethical guidelines and legal frameworks provide guidance for these complex decisions, balancing the principles of autonomy and beneficence.
Ethical Issues in Reflection
Importance of Ethical Reflection
Ethical reflection is a critical component of ethical decision-making in healthcare. It involves systematically considering ethical principles, values, and potential consequences of interventions and decisions. Through ethical reflection, healthcare professionals can enhance their ethical sensitivity, identify potential ethical issues, and make more informed and ethically sound decisions.
Improving Decision-Making and Patient Care
Ethical reflection can significantly improve decision-making and patient care. By critically examining the ethical implications of interventions, healthcare professionals can identify potential conflicts, consider alternative options, and make choices that align with patient values and ethical principles. This leads to more patient-centered and ethically responsible healthcare practices.
Role of Ethics Committees and Ethics Consultations
Ethics committees and ethics consultations provide valuable support for ethical reflection in healthcare. These committees are composed of healthcare professionals, ethicists, and other experts who review complex ethical cases and provide guidance to healthcare teams. Ethics consultations offer a structured process for healthcare professionals to discuss ethical concerns, explore different perspectives, and make ethically informed decisions.
Case Studies and Examples
Informed Consent in Research
In clinical research, obtaining informed consent from participants is essential. A case study could involve a patient who participates in a research trial without fully understanding the risks and benefits of the intervention. This case would highlight the importance of providing clear and comprehensive information to patients before they consent to participate in research.
Confidentiality and Data Breaches, Intervention and reflection basic issues in bioethics 10th edition
A case study could explore the ethical implications of a data breach in a healthcare setting. This could involve the unauthorized access or disclosure of patient medical records, highlighting the importance of maintaining patient confidentiality and protecting sensitive health information.
Emerging Ethical Challenges
Genetic Testing and Discrimination
Advances in genetic testing raise ethical concerns about potential discrimination based on genetic information. A case study could discuss the ethical implications of using genetic information in employment, insurance, or healthcare decisions.
Artificial Intelligence in Healthcare
Artificial intelligence (AI) is increasingly used in healthcare, but its ethical implications need to be carefully considered. A case study could explore the ethical challenges of AI in decision-making, patient privacy, and accountability for outcomes.
User Queries
What is the significance of patient autonomy in bioethics?
Patient autonomy is a fundamental principle in bioethics that recognizes the right of individuals to make decisions about their own healthcare, even if those decisions conflict with the recommendations of healthcare professionals.
How does the principle of beneficence guide healthcare professionals?
The principle of beneficence obligates healthcare professionals to act in the best interests of their patients, promoting their well-being and avoiding harm.
What are some ethical challenges faced by healthcare providers?
Healthcare providers may face ethical challenges such as obtaining informed consent, maintaining patient confidentiality, and making decisions about withdrawing or withholding life-sustaining treatment.